Colorectal Cancer Screening
Colorectal cancer is cancer in the colon or rectum. It's a leading cause of cancer deaths in the U.S. But when this cancer is found and removed early, the chances of a full recovery are very good. Because colorectal cancer rarely causes symptoms in its early stages, screening for the disease is important. It’s even more crucial if you have risk factors for the disease. Learn more about colorectal cancer and its risk factors. Then talk to your healthcare provider about being screened.
Risk factors for colorectal cancer
Your risk of having colorectal cancer increases if you:
-
Are 50 years of age or older, but it can occur in people younger than 50
-
Have a family history or personal history of colorectal cancer or polyps
-
Have a personal history of type 2 diabetes, Crohn’s disease, or ulcerative colitis
-
Have an inherited genetic syndrome like Lynch syndrome (HNPCC) or familial adenomatous polyposis (FAP)
-
Are very overweight
-
Are not physically active
-
Smoke
-
Drink a lot of alcohol
-
Eat a lot of red or processed meat
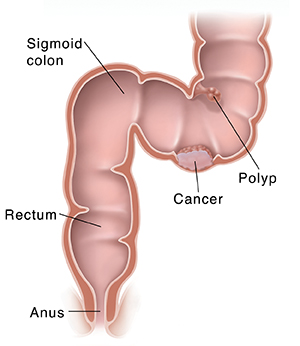
The colon and rectum
Waste from food you eat enters the colon from the small intestine. As it travels through the colon, the waste (stool) loses water and becomes more solid. Intestinal muscles push it toward the sigmoid colon. This is the last section of the colon. Stool then moves into the rectum, where it’s stored until it’s ready to leave the body during a bowel movement.
How colorectal cancer starts
Polyps are growths that form on the inner lining of the colon or rectum. Most are benign, which means they aren’t cancer. But over time, some polyps can become cancer (malignant). This happens when cells in these polyps start growing abnormally. In time, malignant cells invade more of the colon and rectum. The cancer may also spread to nearby organs or lymph nodes or to other parts of the body. Finding and removing polyps can help prevent cancer from forming.
Your screening
Screening means looking for a health problem before you have symptoms. During screening for colorectal cancer, your healthcare provider will ask about your health history, examine you, and do 1 or more tests. To start, you may have:
-
Health history questions to answer. Your healthcare provider will ask about your health history. Mention if a family member has had colon cancer or polyps. Also mention any health problems you have had in the past.
-
Digital rectal exam (DRE). During a DRE, the healthcare provider inserts a lubricated gloved finger into the rectum. The test is painless and takes less than a minute. This test alone is not enough to screen for colorectal cancer. You will also need one of the below tests.
Screening test choices
Some expert groups generally advise that people at average risk for colorectal cancer start screening at age 50.
For those who are 50 years old and of average risk for colorectal cancer, Gundersen Health System (GHS) offers:
-
A colonoscopy every 10 years, or
-
Fecal immunochemical test (FIT) every year, or
-
A stool DNA test every 3 years (Cologuard®)
If you have a family history of colon cancer or are at high risk for other reasons, you may need to have screening even earlier. Talk with your provider to find out about your risk factors.
Colonoscopy
This test can be used to find and remove polyps anywhere in the colon or rectum.
The day before the test, you will do a bowel prep. This is a liquid diet plus a strong laxative solution or an enema. The bowel prep will cleanse your colon. You will be given instructions for this.
Just before the test, you are given a medicine to make you sleepy. Then the healthcare provider gently puts a long, flexible, lighted tube (colonoscope) into your rectum and guides it through the entire colon. The provider looks at images of the colon on a video screen. Any polyps that are found are removed and sent to a lab for testing. If a polyp can’t be removed, a sample of tissue is taken. The polyp might be removed later during surgery.
You will need to bring someone with you to drive you home after this test.
Colonoscopy is the only screening test that lets your healthcare provider see the entire colon and rectum. This test also lets your healthcare provider remove any pieces of tissue that need to be looked at by a lab. If something suspicious is found using any other tests, you will likely need a colonoscopy.
Fecal immunochemical test (FIT)
This test checks for blood in stool that you can’t see (hidden or occult blood). Hidden blood may be a sign of colon polyps or cancer. A small sample of stool is tested for blood in a lab. Most often, you collect this sample at home using a kit your healthcare provider gives you. Follow the instructions carefully for using this kit. You might need to not eat certain foods and not take certain medicines before the test, as directed.
Stool DNA test (Cologuard®)
This test looks for DNA changes in cells in the stool. These DNA changes might be signs of cancer. It also looks for hidden blood in stool. For this test, you collect an entire bowel movement. This is done using a special container put in the toilet. The sample is then sent to a lab for testing.
Talking with your healthcare provider
Talk with your healthcare provider about which tests might be right for you. No matter which test you choose, the most important thing is that you get screened. Keep in mind that if cancer is found at an early stage during screening, treatment is more likely to work well. Many cancers can even be prevented with these tests.
Note: If you choose a test other than a colonoscopy and have an abnormal test result, you will need to follow-up with colonoscopy.
Some people should be screened using a different schedule because of their personal or family history of colorectal cancer. They may also need a different schedule because of polyps or certain inherited conditions. These include familial adenomatous polyposis (FAP), Lynch syndrome (hereditary non-polyposis colon cancer, HNPCC), or inflammatory bowel disease such as Crohn's or ulcerative colitis. Talk with your doctor about your health history.
When to call your healthcare provider after a test
Call your healthcare provider if you have any of the following after any screening test:
All rights reserved - Gundersen Health System Patient Education - This information is meant to inform and educate our patients. It supports the care you receive from your health care team. It does not replace medical evaluation, advice, diagnosis or treatment. Talk to your doctor or health care team before starting any new treatment. Last revised 01/23/2020 PE 002793