Endoscopic Ultrasound (EUS)
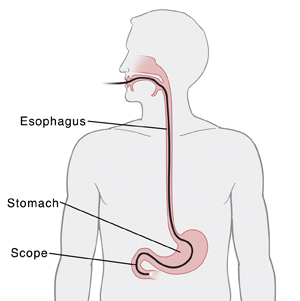
An endoscopic ultrasound (EUS) is a test to look at the inside of your gastrointestinal (GI) tract. It's commonly used to look for cancers or growths in the esophagus, stomach, pancreas, liver, and rectum. It can help to stage cancer (see how advanced a cancer is). EUS may also be used to help diagnose certain diseases or to drain cysts or abscesses.
What is EUS?
EUS shows both ultrasound images and live video of the GI tract. During the test, a flexible tube called an endoscope (scope) is used. At the end of the scope is a tiny video camera and light. The video camera sends live images to a monitor. The scope also contains a very small ultrasound device. This uses sound waves to create images and send them to a monitor.
A needle is passed through the scope. The needle can be used take a small sample of tissue for testing. This is called a biopsy. The needle can be used to take a sample of fluid. This is called fine-needle aspiration (FNA).
Risks and possible complications of EUS
Risks and possible complications include the following:
Before the test
Be prepared prior to the test:
-
Tell your healthcare provider what medicine you take. This includes vitamins, herbs, and over-the-counter medicine. It also includes any blood thinners, such as warfarin, clopidogrel, ibuprofen, or daily aspirin. Ask your healthcare provider if you need to stop taking some or all of them before the test.
-
You may be prescribed antibiotics to take before or after the test. This depends on the area being studied and what is done during the test. These medicines help prevent infection.
-
Carefully follow the instructions for preparing for the test to make sure results are accurate. Instructions may include:
-
If you’re having an EUS of the upper GI tract (esophagus, stomach, duodenum, pancreas, liver):
-
If you’re having an EUS of the lower GI tract (rectum):
-
Before the test, do bowel prep as instructed to clean your rectum of stool. This may involve a clear liquid diet and using a laxative (liquid or pills) the night before the test. Or it may mean doing one or more enemas the morning of the test.
-
Do not eat or drink for 6 hours before the test.
-
Be sure to arrive on time at the facility. Bring your identification and health insurance card. Leave valuables at home. If you have them, bring X-rays or other test results with you.
Let the healthcare provider know
For your safety, tell the healthcare provider if you:
-
Take insulin. Your dose may need to be changed on the day of your test.
-
Are allergic to latex.
-
Have any other allergies.
-
Are taking blood thinners.
During the test
An endoscopic ultrasound usually takes place in a hospital. The procedure itself may take 1 to 2 hours. You will likely go home soon afterward. During the test:
-
You lie on your left side on an exam table.
-
An intravenous (IV) line will be put into a vein in your arm or hand. This line supplies fluids and medicines. To keep you comfortable during the test, you will be given a sedative medicine. This medicine prevents discomfort and will make you sleepy.
-
If you are having an EUS of the upper GI tract, local anesthetic may be sprayed in your throat. This will help you be more comfortable as the healthcare provider inserts the scope. The healthcare provider then gently puts the flexible scope into your mouth or nose and down your throat.
-
If you’re having an EUS of the lower GI tract, the healthcare provider gently puts the flexible scope into your anus.
-
During the test, the scope sends live video and ultrasound images from inside your body to nearby monitors. These are used to examine your GI tract. Specialized procedures, such as drainage, are done as needed.
-
The healthcare provider may discuss the results with you soon after the test. Biopsy results take several days.
-
In most cases, you can go home within a few hours of the test. When you leave the facility, have an adult family member or friend drive you, even if you don't feel that sleepy.
After the test
Here is what to expect after the test:
-
You may feel tired from the sedative. This should wear off by the end of the day.
-
If you had an upper digestive endoscopy, your throat may feel sore for a day or two. Over-the-counter sore throat lozenges and spray should help.
-
You can eat and drink normally as soon as the test is done.
When to call the healthcare provider
Call your healthcare provider if you notice any of the following:
-
Fever of 100.4°F (38.0°C) or higher, or as advised by your healthcare provider
-
Shortness of breath
-
Vomiting blood, blood in stool, or black stools
-
Coughing or hoarse voice that won’t go away
Endoscopic Ultrasound (EUS)
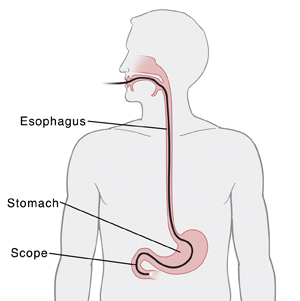
An endoscopic ultrasound (EUS) is a test to look at the inside of your gastrointestinal (GI) tract. It's commonly used to look for cancers or growths in the esophagus, stomach, pancreas, liver, and rectum. It can help to stage cancer (see how advanced a cancer is). EUS may also be used to help diagnose certain diseases or to drain cysts or abscesses.
What is EUS?
EUS shows both ultrasound images and live video of the GI tract. During the test, a flexible tube called an endoscope (scope) is used. At the end of the scope is a tiny video camera and light. The video camera sends live images to a monitor. The scope also contains a very small ultrasound device. This uses sound waves to create images and send them to a monitor.
A needle is passed through the scope. The needle can be used take a small sample of tissue for testing. This is called a biopsy. The needle can be used to take a sample of fluid. This is called fine-needle aspiration (FNA).
Risks and possible complications of EUS
Risks and possible complications include the following:
Before the test
Be prepared prior to the test:
-
Tell your healthcare provider what medicine you take. This includes vitamins, herbs, and over-the-counter medicine. It also includes any blood thinners, such as warfarin, clopidogrel, ibuprofen, or daily aspirin. Ask your healthcare provider if you need to stop taking some or all of them before the test.
-
You may be prescribed antibiotics to take before or after the test. This depends on the area being studied and what is done during the test. These medicines help prevent infection.
-
Carefully follow the instructions for preparing for the test to make sure results are accurate. Instructions may include:
-
If you’re having an EUS of the upper GI tract (esophagus, stomach, duodenum, pancreas, liver):
-
If you’re having an EUS of the lower GI tract (rectum):
-
Before the test, do bowel prep as instructed to clean your rectum of stool. This may involve a clear liquid diet and using a laxative (liquid or pills) the night before the test. Or it may mean doing one or more enemas the morning of the test.
-
Do not eat or drink for 6 hours before the test.
-
Be sure to arrive on time at the facility. Bring your identification and health insurance card. Leave valuables at home. If you have them, bring X-rays or other test results with you.
Let the healthcare provider know
For your safety, tell the healthcare provider if you:
-
Take insulin. Your dose may need to be changed on the day of your test.
-
Are allergic to latex.
-
Have any other allergies.
-
Are taking blood thinners.
During the test
An endoscopic ultrasound usually takes place in a hospital. The procedure itself may take 1 to 2 hours. You will likely go home soon afterward. During the test:
-
You lie on your left side on an exam table.
-
An intravenous (IV) line will be put into a vein in your arm or hand. This line supplies fluids and medicines. To keep you comfortable during the test, you will be given a sedative medicine. This medicine prevents discomfort and will make you sleepy.
-
If you are having an EUS of the upper GI tract, local anesthetic may be sprayed in your throat. This will help you be more comfortable as the healthcare provider inserts the scope. The healthcare provider then gently puts the flexible scope into your mouth or nose and down your throat.
-
If you’re having an EUS of the lower GI tract, the healthcare provider gently puts the flexible scope into your anus.
-
During the test, the scope sends live video and ultrasound images from inside your body to nearby monitors. These are used to examine your GI tract. Specialized procedures, such as drainage, are done as needed.
-
The healthcare provider may discuss the results with you soon after the test. Biopsy results take several days.
-
In most cases, you can go home within a few hours of the test. When you leave the facility, have an adult family member or friend drive you, even if you don't feel that sleepy.
After the test
Here is what to expect after the test:
-
You may feel tired from the sedative. This should wear off by the end of the day.
-
If you had an upper digestive endoscopy, your throat may feel sore for a day or two. Over-the-counter sore throat lozenges and spray should help.
-
You can eat and drink normally as soon as the test is done.
When to call the healthcare provider
Call your healthcare provider if you notice any of the following:
-
Fever of 100.4°F (38.0°C) or higher, or as advised by your healthcare provider
-
Shortness of breath
-
Vomiting blood, blood in stool, or black stools
-
Coughing or hoarse voice that won’t go away